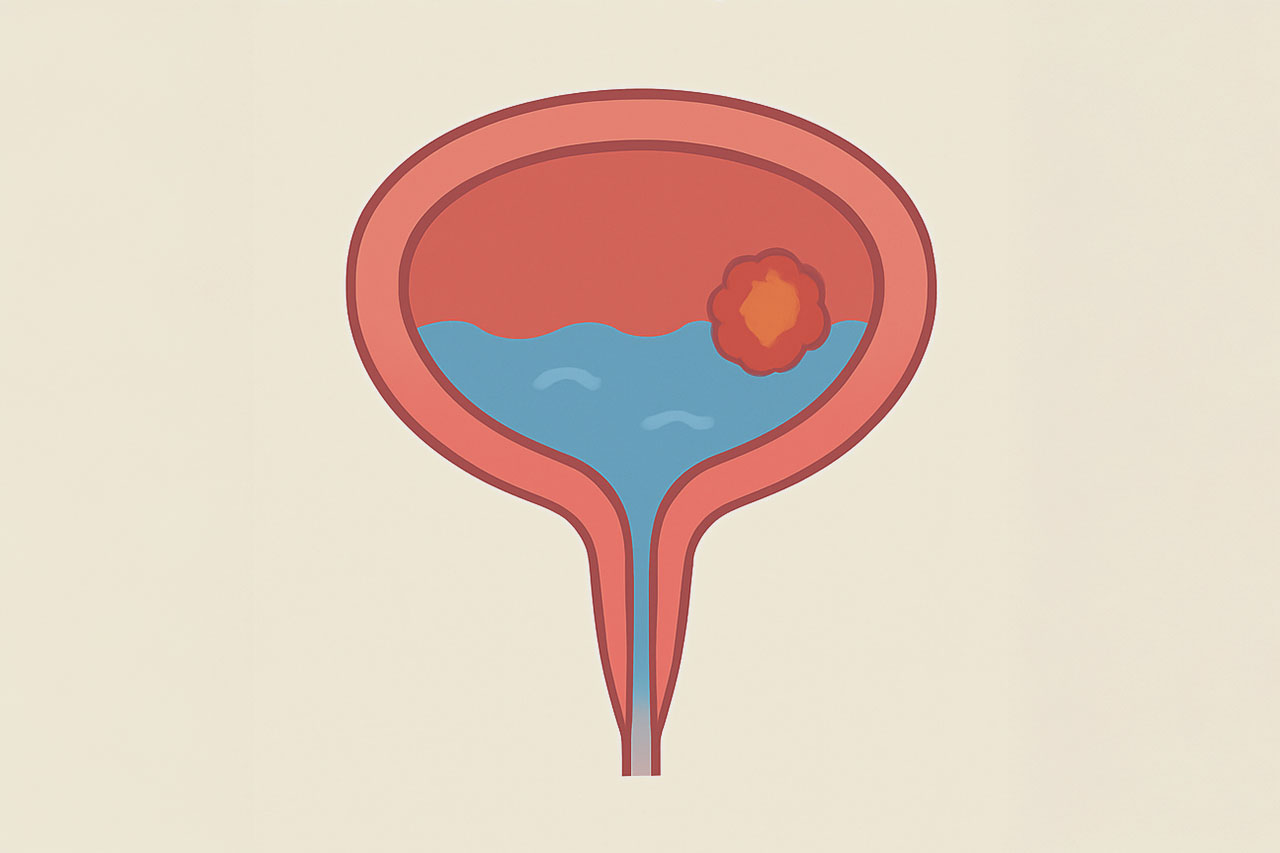
Bladder Cancer
Harley Street, London
Bladder cancer arises from the urothelial cells that line the bladder. It can manifest in various forms and stages, significantly influencing treatment decisions and outcomes.
Types of Bladder Cancer:
- Non-Muscle Invasive Bladder Cancer (NMIBC):
- Stage Ta: Tumors are confined to the bladder lining (mucosa).
- Stage T1: Tumors invade the connective tissue beneath the bladder lining but do not reach the muscle layer.
- Carcinoma In Situ (CIS): Flat, high-grade tumors that are also confined to the bladder lining.
- Muscle-Invasive Bladder Cancer (MIBC):
- Stage T2: Tumors invade the muscle layer of the bladder.
- Stage T3: Tumors extend through the bladder wall and may invade surrounding tissues.
- Stage T4: Tumors spread to nearby organs (e.g., prostate, uterus) or lymph nodes.
Symptoms
- Haematuria: The most common symptom, often painless, indicating the presence of a tumor.
- Dysuria: Painful urination or a burning sensation.
- Increased Urgency and Frequency: A need to urinate more often, sometimes with little urine output.
- Pelvic Pain: Discomfort or pain in the lower abdomen, which may indicate advanced disease.
- Weight Loss and Fatigue: Unexplained weight loss and persistent fatigue can occur in more advanced stages.
Diagnosis
The diagnostic process is crucial for determining the appropriate treatment plan. It typically involves:
- Medical History and Physical Examination: A detailed review of symptoms, medical history, and family history of cancer.
- Cystoscopy: A key diagnostic procedure where a thin, lighted tube (cystoscope) is inserted through the urethra to visualise the bladder. The procedure is usually performed under local anaesthetic.
- Imaging Studies:
- CT Urography: Provides detailed images of the urinary tract, helping to identify tumors in the kidneys and ureters.
- MRI: Useful for assessing the extent of muscle invasion and checking for spread to nearby tissues and lymph nodes.
- PET Scan: Sometimes used to evaluate for metastasis by highlighting areas of increased metabolic activity.
Treatment Options
Mr. Raison offers a multidisciplinary approach to bladder cancer treatment, considering the specific characteristics of the tumour and the patient’s overall health.
Treatment of Non-Muscle Invasive Bladder Cancer (NMIBC)
Non-muscle invasive bladder cancer (NMIBC) is characterised by tumors that have not invaded the muscle layer of the bladder wall. The treatment approach for NMIBC typically involves a combination of surgical intervention and intravesical therapy. Here are the main treatment options:
Transurethral Resection of Bladder Tumor (TURBT)
- Procedure: TURBT is the primary treatment for NMIBC. It involves the removal of visible tumors from the bladder using a cystoscope, which is inserted through the urethra. This procedure allows for both diagnosis and treatment.
- Goals: The main goals are to remove the tumour completely and to obtain tissue samples for histological analysis to determine the tumour’s grade and stage.
Intravesical Therapy
After TURBT, patients with NMIBC often receive intravesical therapy to reduce the risk of recurrence. This involves administering medication directly into the bladder through a catheter.
The two main types of intravesical therapy are:
- Intravesical Chemotherapy:
- Agents Used: Common agents include mitomycin C, doxorubicin, and epirubicin.
- Schedule: Typically administered once a week for 6-8 weeks following TURBT. Maintenance therapy may be recommended based on individual risk factors.
- Mechanism: Chemotherapy works by killing cancer cells and preventing them from growing back.
- Intravesical Immunotherapy:
- BCG Therapy (Bacillus Calmette-Guérin): This is the most effective form of immunotherapy for NMIBC.
- Administration: BCG is instilled into the bladder once a week for 6 weeks, followed by maintenance doses (usually every 3-6 months) for up to 3 years.
- Mechanism: BCG stimulates the immune system to attack cancer cells in the bladder, reducing the risk of recurrence and progression.
- BCG Therapy (Bacillus Calmette-Guérin): This is the most effective form of immunotherapy for NMIBC.
Follow-Up and Surveillance
- Cystoscopy: Regular follow-up cystoscopies are essential for monitoring recurrence. The frequency of cystoscopy typically starts at every 3-6 months for the first few years after treatment, then may be extended based on individual risk factors.
- Urinary Cytology: In some cases, urine tests may be performed to check for cancer cells, although cystoscopy remains the gold standard for surveillance.
Considerations for Treatment
- Risk Stratification: Treatment decisions are influenced by the tumor’s characteristics, including stage (Ta, T1, CIS), grade (low vs. high), and the presence of multiple tumors or prior recurrences.
- Patient Factors: Overall health, preferences, and potential side effects of treatments are also considered when developing a treatment plan.
Treatment of Muscle-Invasive Bladder Cancer (MIBC)
Muscle-invasive bladder cancer (MIBC) is characterised by tumors that have penetrated the muscle layer of the bladder wall. The treatment approach for MIBC typically involves a combination of surgical and systemic therapies. Here’s a summary of the main treatment options:
Surgical Treatment
- Radical Cystectomy: The primary treatment for MIBC is the surgical removal of the entire bladder (cystectomy) along with surrounding tissues and possibly nearby lymph nodes. In men, this may also include the removal of the prostate, and in women, the removal of the uterus and ovaries may be necessary.
- Urinary Diversion: After cystectomy, a new way to store urine must be created, which can involve creating a neobladder or using an external pouch.
Neoadjuvant Chemotherapy
- Purpose: Chemotherapy may be administered before surgery (neoadjuvant chemotherapy) to shrink the tumour and improve surgical outcomes.
- Common Regimens: Platinum-based chemotherapy regimens, such as MVAC (methotrexate, vinblastine, doxorubicin, and cisplatin) or gemcitabine and cisplatin, are commonly used.
Adjuvant Chemotherapy
- Post-Surgery Treatment: After surgery, adjuvant chemotherapy may be recommended to eliminate any remaining cancer cells and reduce the risk of recurrence.
Bladder-Sparing Approaches
- Consideration for Selected Patients: In some cases, a bladder-sparing approach may be considered, which involves a combination of TURBT, chemotherapy, and radiation therapy. This is typically reserved for patients who are not candidates for radical cystectomy or prefer to preserve bladder function.
Follow-Up and Surveillance
- Regular Monitoring: After treatment, patients require ongoing follow-up to monitor for recurrence, which may include cystoscopy and imaging studies.
Follow-Up Care
Post-treatment follow-up is critical for monitoring recurrence and managing any long-term effects of treatment. Mr. Raison emphasises:
- Regular Cystoscopies: Typically performed every 3-6 months for the first few years after treatment to check for recurrence.
- Imaging Studies: Periodic CT or MRI scans to monitor for metastasis, especially in muscle-invasive cases.
- Symptom Management: Addressing any side effects from treatment, such as urinary incontinence or changes in bladder function.
Mr Raison is available for private urology consultations, treatments, and surgical procedures at The London Clinic, Harley Street.
